Drivers of Prurigo Nodularis
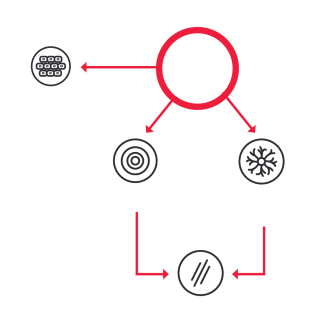
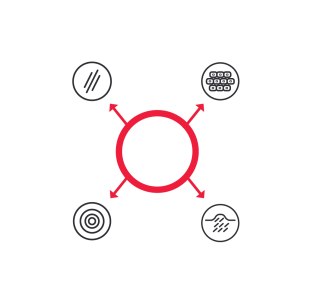
Itch, inflammation, altered epidermal differentiation, and fibrosis contribute to PN.
The pathophysiology of PN involves interactions between the nervous system, immune system, and skin.1-5
Chronic itch results from a complex interplay among T cells, mast cells, neutrophils, eosinophils, keratinocytes, and nerve cells (along with increased release of cytokines, proteases, and neuropeptides), leading to exacerbation of itch.6
Itch sensitization is remarkable to PN pathophysiology and is what distinguishes patients with PN.
Overactivation of the immune system induces inflammation and sensitizes sensory neurons to pruritogens.7-12
A study of patients with chronic inflammatory skin diseases showed that the highest levels of IL-31 were located in lesions of individuals with PN (50-fold higher than in the skin of healthy individuals).13
In mice studies, overexpression of IL-31 was associated with sensory neuronal outgrowth, providing increased sensitivity to minimal itch-inducing stimuli.8
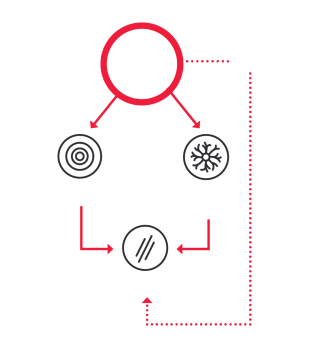
Inflammation contributes to PN pathophysiology.
- Overactivated neurons, in turn, produce inflammatory cytokines, stimulating the recruitment of inflammatory cells7,15-17
- IL-31 contributes to neuroimmune cross talk between fibroblasts, keratinocytes, and the nervous and immune systems17-19
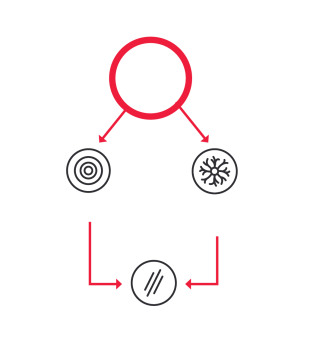
Altered epidermal differentiation contributes to PN pathophysiology.
- Keratinocyte differentiation and activation of fibroblasts are involved in skin integrity and tissue remodeling, respectively19,20
- IL-31 contributes to altered epidermal differentiation by inducing proinflammatory effects of keratinocytes and modulating keratinocyte differentiation 7,18,20-27
- Inhibiting IL-31 signaling results in normalized epidermal hyperproliferation and differentiation7
Fibrosis contributes to PN pathophysiology.
- Lesions associated with PN show fibrosis of the papillary dermis, hypergranulosis, irregular hyperplasia, orthohyperkeratosis, and an increased number of fibroblasts and capillaries7
- Fibrosis is believed to play a role in the pathophysiology of PN, although other interleukins, such as IL-4, IL-17, and IL-22, may also contribute7,14
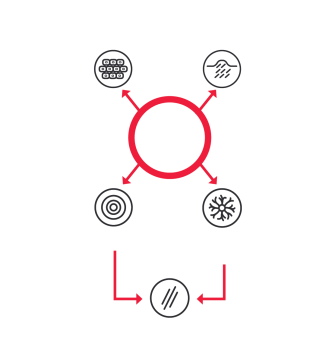
- IL-31 acts as a bridge in PN connecting immune cells, neurons, and structural cells in the skin15,23,29-31
- PN transcriptomic analysis shows that PN is a distinct disease with a unique molecular signature7
- Ständer S, Pereira MP, Berger T, et al. IFSI-guideline on chronic prurigo including prurigo nodularis. Itch. 2020;5(4):e42. doi:10.1097/itx.0000000000000042
- Zeidler C, Pereira M, Ständer S. The neuromodulatory effect of antipruritic treatment of chronic prurigo. Dermatol Ther (Heidelb). 2019;9(4):613-622. doi:10.1007/s13555-019-00321-6
- Hughes JM, Woo TE, Belzberg M, et al. Association between prurigo nodularis and etiologies of peripheral neuropathy: suggesting a role for neural dysregulation in pathogenesis. Medicines (Basel). 2020;7(1):4. doi:10.3390/medicines7010004
- Bewley A, Homey B, Pink A. Prurigo nodularis: a review of IL-31RA blockade and other potential treatments. Dermatol Ther (Heidelb). 2022;12(9):2039-2048. doi: 10.1007/s13555-022-00782-2
- Weigelt N, Metze D, Ständer S. Prurigo nodularis: systematic analysis of 58 histological criteria in 136 patients. J Cutan Pathol. 2010;37(5):578-586. doi:10.1111/j.1600-0560.2009.01484.x
- Yosipovitch G, Bernhard JD. Chronic pruritis. N Engl J Med. 2013;368(17):1625-1634. doi:10.1056/NEJMcp1208814
- Williams KA, Huang AH, Belzberg M, Kwatra SG. Prurigo nodularis: pathogenesis and management. J Am Acad Dermatol. 2020;83(6):1567-1575. doi:10.1016/j.jaad.2020.04.182
- Feld M, Garcia R, Buddenkotte J, et al. The pruritus- and TH2-associated cytokine IL-31 promotes growth of sensory nerves. J Allergy Clin Immunol.2016;138(2):500-508.e24. doi:10.1016/j.jaci.2016.02.020
- Mack MR, Kim BS. The itch-scratch cycle: a neuroimmune perspective. Trends Immunol. 2018;39(12):980-991. doi:10.1016/j.it.2018.10.001
- Ständer S. Atopic dermatitis. N Engl J Med. 2021;384(12):1136-1143. doi:10.1056/NEJMra2023911
- Tominaga M, Takamori K. Peripheral itch sensitization in atopic dermatitis. Allergol Int. 2022;71(3):265-277. doi:10.1016/j.alit.2022.04.003
- Vaalasti A, Suomalainen H, Rechardt L. Calcitonin gene-related peptide immunoreactivity in prurigo nodularis: a comparative study with neurodermatitis circumscripta. Br J Dermatol. 1989;120(5):619-623. doi:10.1111/j.1365-2133.1989.tb01346.x
- Sonkoly E, Muller A, Lauerma AI, et al. IL-31: a new link between T cells and pruritus in atopic skin inflammation. J Allergy Clin Immunol. 2006;117:411-417. doi: 10.1016/j.jaci.2005.10.033
- Datsi A, Steinhoff M, Ahmad F, Alam M, Buddenkotte J. Interleukin-31: The “itchy” cytokine in inflammation and therapy. Allergy. 2021;76(10):2982-2997. doi:10.1111/all.14791
- Wang F, Kim BS. Itch: a paradigm of neuroimmune crosstalk. Immunity. 2020;52(5):753-766. doi:10.1016/j.immuni.2020.04.008
- Zeidler C, Yosipovitch G, Ständer S. Prurigo nodularis and its management. Dermatol Clin. 2018;36(3):189-197. doi:10.1016j.det.2018.02.003
- Agelopoulos K, Pereira MP, Wiegmann H, Ständer S. Cutaneous neuroimmune crosstalk in pruritus. Trends Mol Med. 2022;28(6):452-462. doi:10.1016/j.molmed.2022.03.005
- Gibbs BF, Patsinakidis N, Raap U. Role of the pruritic cytokine IL-31 in autoimmune skin diseases. Front Immunol. 2019;10:1383. doi:10.3389/fimmu.2019.01383
- Di Salvo E, Ventura-Spagnolo E, Casciaro M, Navarra M, Gangemi S. IL-33/IL-31 axis: a potential inflammatory pathway. Mediators Inflamm. 2018;2018:3858032. doi:10.1155/2018/3858032
- Kuzumi A, Yoshizaki A, Matsuda KM, K, et al. Interleukin-31 promotes fibrosis and T helper 2 polarization in systemic sclerosis. Nat Commun. 2021;12(1):5947. doi:10.1038/s41467-021-26099-w
- Cornelissen C, Marquardt Y, Czaja K, et al. IL-31 regulates differentiation and filaggrin expression in human organotypic skin models. J Allergy Clin Immunol. 2012;129(2):426–433.e4338. doi:10.1016/j.jaci.2011.10.042
- Singh B, Jegga AG, Shanmukhappa KS, et al. IL-31-driven skin remodeling involves epidermal cell proliferation and thickening that lead to impaired skin-barrier function. PloS One. 2016;11(8):e0161877. doi:10.1371/journal.pone.0161877
- Bagci IS, Ruzicka T. IL-31: A new key player in dermatology and beyond. J Allergy Clin Immunol. 2018;141(3):858-866. doi:10.1016/j.jaci.2017.10.045
- Kabashima K, Irie H. Interleukin-31 as a clinical target for pruritus treatment. Front Med (Lausanne). 2021;8:69. doi:10.3389/fmed.2021.638325
- Chaowattanapanit S, Wongjirattikarn R, Chaisuriya N, et al. Increased IL-31 expression in serum and tissue protein in prurigo nodularis.Ther Adv Chronic Dis. 2022;13:20406223221112561. doi: 10.1177/20406223221112561
- Yombo DJK, Odayar V, Gupta N, Jegga AG, Madala SK. The protective effects of IL-31RA deficiency during bleomycin-induced pulmonary fibrosis. Front Immunol. 2021;12:682. doi:10.3389/fimmu.2021.645717
- Wong CK, Leung KM, Qiu HN, et al. Activation of eosinophils interacting with dermal fibroblasts by pruritogenic cytokine IL-31 and alarmin IL-33: implications in atopic dermatitis. PLoS One. 2012;7(1):e29815. doi:10.1371/journal.pone.0029815
- Williams KA, Roh YS, Brown I, et al. Pathophysiology, diagnosis, and pharmacological treatment of prurigo nodularis. Expert Rev Clin Pharmacol. 2021;14(1):67-77. doi:10.1080/17512433.2021.1852080
- Zhang Q, Putheti P, Zhou Q, Liu Q, Gao W. Structures and biological functions of IL-31 and IL-31 receptors. Cytokine Growth Factor Rev. 2008;19(5-6):347-356. doi:10.1016/j.cytogfr.2008.08.003
- Furue M, Furue M. Interleukin-31 and pruritic skin. J Clin Med. 2021;10(9):1906. doi:10.3390/jcm10091906
- Sutaria N, Alphonse MP, Roh YS, et al. Cutaneous transcriptomics identifies fibroproliferative and neurovascular gene dysregulation in prurigo nodularis compared with psoriasis and atopic dermatitis. J Invest Dermatol. 2022;142(9):2537-2540. doi:10.1016/j.jid.2022.02.010